Prostate cancer study focuses on new drug therapy
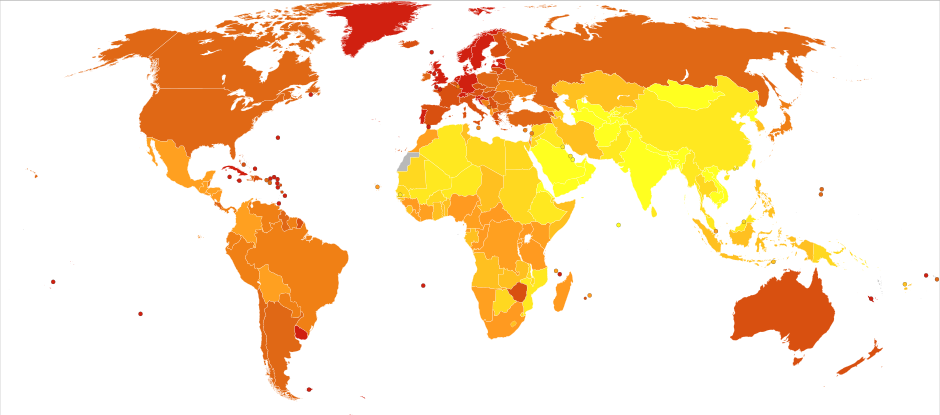
Deaths from prostate cancer in 2012 per million males. Statistics from WHO, grouped by deciles, show that the U.S. and Canada have some of the highest rates of prostate cancer deaths. (Wikimedia)
There are roughly 3,400 new cases of prostate cancer diagnosed in Maryland each year, making it the third most common form of cancer in the state. Most believe prostate cancer is something men die with, not from, but in some cases, it can advance and become life-threatening.
Chesapeake Urology in Baltimore, Maryland, is participating in a national clinical trial program for (the ongoing Phase III ARASENS trial) investigating darolutamide, a novel investigational therapy, to potentially delay mHSPC progression. To better understand the prostate cancer and the aims of the study, we contacted Dr. Ronald F. Tutrone, Jr.: Chief, Division of Urology, Greater Baltimore Medical Center, and Medical Director at Chesapeake Urology Research Associates. Tutrone talks here about the clinical trial and shares information on what to do when facing a mHSPC diagnosis.
BPE: Please walk us through a diagnosis of prostate cancer. What symptoms do patients present and what are doctors looking for?
Tutrone: In my experience, most patients who have prostate cancer present with no symptoms and are typically referred to a urologist because they may have high PSA (prostate-specific antigen) levels. Some patients may see blood in their semen or have urinary complaints such as frequency, slowing of their stream or blood in their urine. Rarely patients may present with bone pain due to metastatic disease.
As a urologist, one screening method we use tests the levels of PSA, and we make sure to look out for any sharp rises in PSA levels. More important than the absolute PSA value is it’s change over time or velocity.
BPE: How many Marylanders die annually from prostate cancer?

Tutrone: According to the National Cancer Institute, more than 4,000 people in Maryland die from prostate cancer each year.
BPE: How critical is early diagnosis and treatment?
Tutrone: Early diagnosis and treatment are key because if you are able to detect the cancer early, the odds of curing the patient with therapy, are greatly improved.
BPE: What traditional treatments are available? And how successful are those treatments?
Tutrone: Within our practice, we treat a lot of prostate cancer cases by putting patients on active surveillance and do not give them definitive therapy upfront. The patients who are ideal candidates for active surveillance are patients that have low risk, low volume, low grade prostate cancer. Most of these patients will die with the disease rather than from it.
Patients who have a higher risk, higher grade cancer who have at least a five-year life expectancy may choose surgical removal of the prostate or radiation. In patients whose cancer is not localized to the prostate, or advanced, such as those with bone metastases or lymph node metastases, we usually treat them upfront with hormonal therapy.
The success of the treatment depends on the stage of the tumor. If a patient has localized prostate cancer and they are treated with radiation or surgery, they have a better than 90 percent chance for 10-year survival. But in patients with a higher grade and a higher stage of cancer, the long-term survival rate drops.
If a patient has metastases to the bones or lymph nodes, the cancer is not curable and a percentage of those patients will have progressive disease in five years. Fifty percent of patients will develop what is called castration-resistant prostate cancer after five years, which means that PSA will start rising and the cancer will start growing despite them having castrate level testosterone.
BPE: Is there a link between testosterone and the development of prostate cancer? If so, what do we know about that link?

Tutrone: We know that testosterone itself does not cause prostate cancer. But it is important to note that prostate cancer cells have testosterone receptors that when exposed to testosterone, are stimulated to grow.
Prostate cancer cells depend on what’s called androgen receptor signaling for their growth and survival, which is activated by binding either of the hormones, testosterone, or dihydrotestosterone. We are continuing to explore therapies that aim to inhibit this activity to prevent or slow the development of prostate cancer.
BPE: Chesapeake Urology in Baltimore, Maryland, is participating in a national clinical trial program investigating darolutamide. How did your group become involved in this study?
Tutrone: I have been involved in studies for over 20 years. My primary goal at Chesapeake Urology is to grow the research program. We offer many clinical trials dealing with prostate cancer from early detection with blood tests and urine tests, to advanced treatments for patients who have failed multiple therapies. I am particularly passionate about it, because within the past seven years there has been huge growth in the different treatment modalities that we can offer patients, ranging from immunotherapy to oral drugs. We have been involved in the development of many of those drugs through clinical trials. You really can’t get those drugs to commercial use unless you have robust, randomized clinical trials.
Darolutamide is an investigational oral androgen receptor antagonist being investigated in prostate cancer. Darolutamide is a second-generation androgen receptor blocker, which means that it blocks the growth of cancer cells by binding to the androgen receptors and preventing testosterone from stimulating cell growth. We are looking to introduce these drugs even earlier in the disease, before patients have metastatic castration-resistant prostate cancer.
A big reason we became involved in the darolutamide clinical trial program, and why we do research, is so we can offer better services and better outcomes for patients. In my experience, clinical trials give patients more control and a better understanding of what they are dealing with. In addition, we are able to follow the patient very closely, so if there is any change in their disease, we can react to those changes sooner and hopefully extend the survival for that patient.
BPE: Are either Chesapeake Urology or members of its staff being remunerated by the manufacturer (Bayer) in any way for this study?

Tutrone: We are contracted to conduct a clinical trial, which is standard practice. As part of the trial protocol, we provide care such as a physician exam for patients, and hire certified clinical research coordinators to monitor the patients and collect the study data.
BPE: What – if any – are the costs to the patient?
Tutrone: Patients are reimbursed for expenses such as travel, gas, parking, etc. in an effort to be sure there are no costs to them for trial participation, outside of regular medical expenses.
BPE: How are patients being selected for this study?
Tutrone: Every trial that we evaluate has what are called inclusion and exclusion criteria upon which you can enter a patient into a trial, which is all overseen by the FDA. Every trial is different. The ARASENS trial studies patients with metastatic hormone-sensitive prostate cancer (mHSPC) who have started androgen deprivation therapy (ADT) combined with chemotherapy and are randomized to also receive darolutamide or placebo.
At Chesapeake Urology, we send quarterly newsletters listing our available trials. We also have a website listing the clinical trials for different conditions for patients to access and carry pamphlets in all of the exam rooms. It’s very important to disseminate that information to all of our caregivers and doctors at CUA, so that when they see a patient in the clinic, they can suggest a potential trial that fits their patient’s condition.
BPE: What can patients who are involved in this study expect? What if any are the risks of being involved?
Tutrone: The first thing I stress to every patient, is that they all undergo the informed consent process, which informs them of their rights. I like to stress to the patient that they always have the right to withdraw consent from the study at any time. On the first day of their visit, we have a screening and give them a consent form to review, which lists all of the risks and side effects of participating in the trial investigating an experimental drug. Patients can expect that we will capture any side effects related to darolutamide, as one of our key purposes is to better understand what those possible side effects – if any – may be.
BPE: What is the length of the ARASENS study?
Tutrone: All clinical trials are event based, but the ARASENS study started in 2016, with expected completion in 2022.
BPE: Does Bayer believe darolutamide may someday benefit patients diagnosed with other kinds of cancer?
Tutrone: Darolutamide is currently being tested for advanced prostate cancer. It is hopeful that darolutamide will show comparable efficacy with less morbidity to some of the other drugs that are on the market, quite extensively used in place of what is out there now for prostate cancer. With many of the clinical trials that we are conducting, we are introducing new drugs that have the potential to be effective earlier in prostate cancer, before patients develop metastatic castrate-resistant prostate cancer.
BPE: If this drug shows promise and the trials are successful, do you have any idea how long it might be before darolutamide is on the market?
Tutrone: With the estimated completion date of ARAMIS and ARASENS studies expected in 2018 and 2022 respectively, I believe the FDA will have the opportunity to review the data closely thereafter.
BPE: Is there anything you’d like to add in closing?
Tutrone: From a 30,000-foot view, prostate cancer research is at least 10 years behind breast cancer research. They are both very similar diseases in that the adenocarcinoma are hormone sensitive – with breast cancer being sensitive to estrogen, and prostate cancer being sensitive to testosterone. There is a great need for funding for prostate cancer research to bring it to the same level of attention as breast cancer.

Anthony C. Hayes is an actor, author, raconteur, rapscallion and bon vivant. A one-time newsboy for the Evening Sun and professional presence at the Washington Herald, Tony’s poetry, photography, humor, and prose have also been featured in Smile, Hon, You’re in Baltimore!, Destination Maryland, Magic Octopus Magazine, Los Angeles Post-Examiner, Voice of Baltimore, SmartCEO, Alvarez Fiction, and Tales of Blood and Roses. If you notice that his work has been purloined, please let him know. As the Good Book says, “Thou shalt not steal.”